It’s not you, it’s me: Framing Conversations About Back Pain
December 11th, 2017 | Clinical Connectionsby Matt Devine, D.O. – AHP Medical Director
Recently, AHP commenced on a new process aimed to help us improve patient care and delivery by becoming more collaborative across the network. (Drumroll…) The AHP back pain committee has become the first integrated practice committee (IPC) in our network. The charge of this committee is to improve the care that we provide to acute back pain patients when they are having this extremely common and usually self-limiting problem. At the AHP October Clinical Grand Rounds I spoke about the care delivery of back pain from a primary care perspective.
When acute back pain develops, the patient’s fear, uncontrolled pain, and concerns about long term health problems often lead to unnecessary testing and treatment. The pain intensity and their concerns offers all of us an opportunity for a “teachable moment.” Different than most chronic conditions, the acute phase of back pain can allow us to work with the patient on his “health bucket list” items which can significantly help improve back pain and overall health. Some of the most success that I have had as a PCP working on strategies for weight loss, tobacco cessation, increasing activity, and stress reduction have occurred when I was able to engage with a patient that presented to me with an acute symptom like back pain. The availability of more time is not necessary to work on these health changes, but it does require finesse when being delivered to the patient. Therefore the dialogue and discussions surrounding the plans are critical. In my discussion at Clinical Grand Rounds I drew upon the research of Dr. Sherri Weiser, an orthopedic surgeon at NYU. She has done a great amount of research into the psychological effects that treating conditions like back pain can have on a patient. She has presented and published tools that can help us to properly frame our discussions in ways that enable the patient to better understand our plans, and dialogue when they are in the throes of their acute episode.
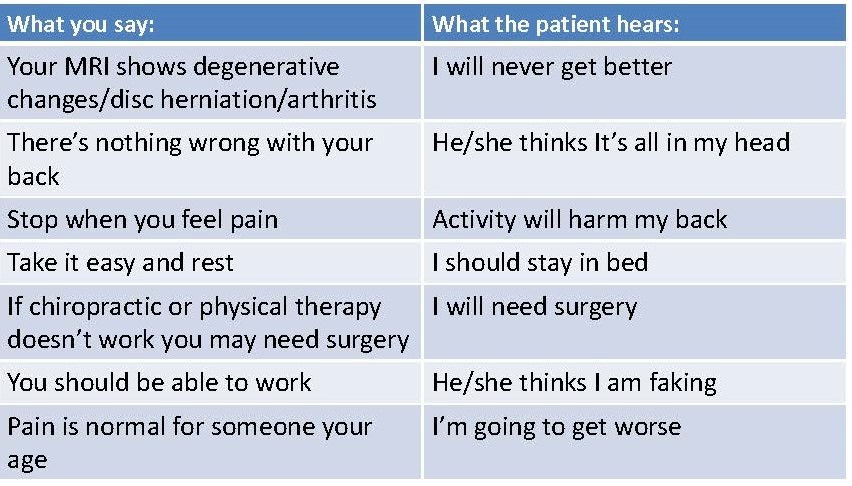
Here are examples of common misconceptions that occur when we discuss back pain with patients in the office in a biomedical manner:
What you say: What the patient hears:
Here are some examples of dialogue that uses a more psychosocial manner to discuss back pain with our patients:
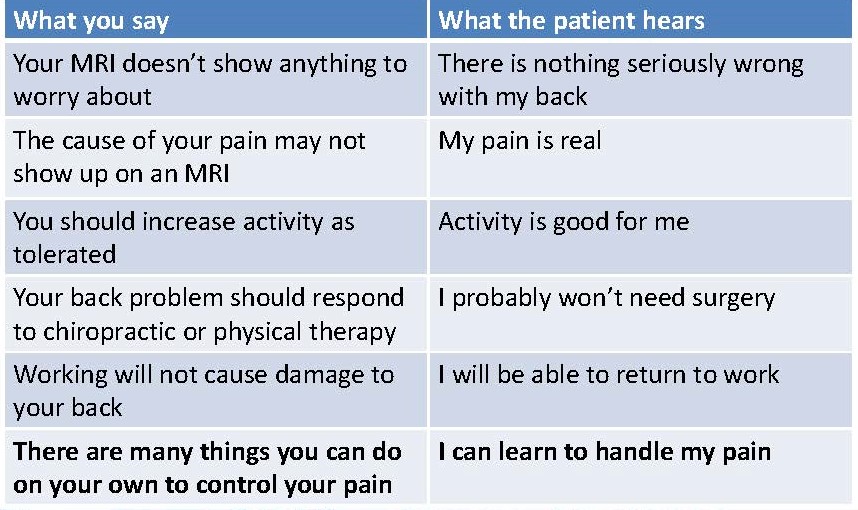
**These slides were used with permission from Sherri Weiser, PhD NYU School of Medicine
This Back Pain IPC is still in its infancy stages. We are looking forward to sharing with you further innovations that will help all clinicians who are treating back pain. If you are interested in participating in or contributing to this IPC, please Melissa Claybaugh or Mathew Devine
















