How are the PHQ 2 and 9 tools used?
The PHQ 2 is a tool used to screen for depression, while the PHQ 9 tool is used to screen or diagnose depression, measure the severity of symptoms, and measure a patient’s response to treatment. The PHQ 2 and 9 are quick and easy to administer1,2.
What is the difference between a PHQ 2 and 9?
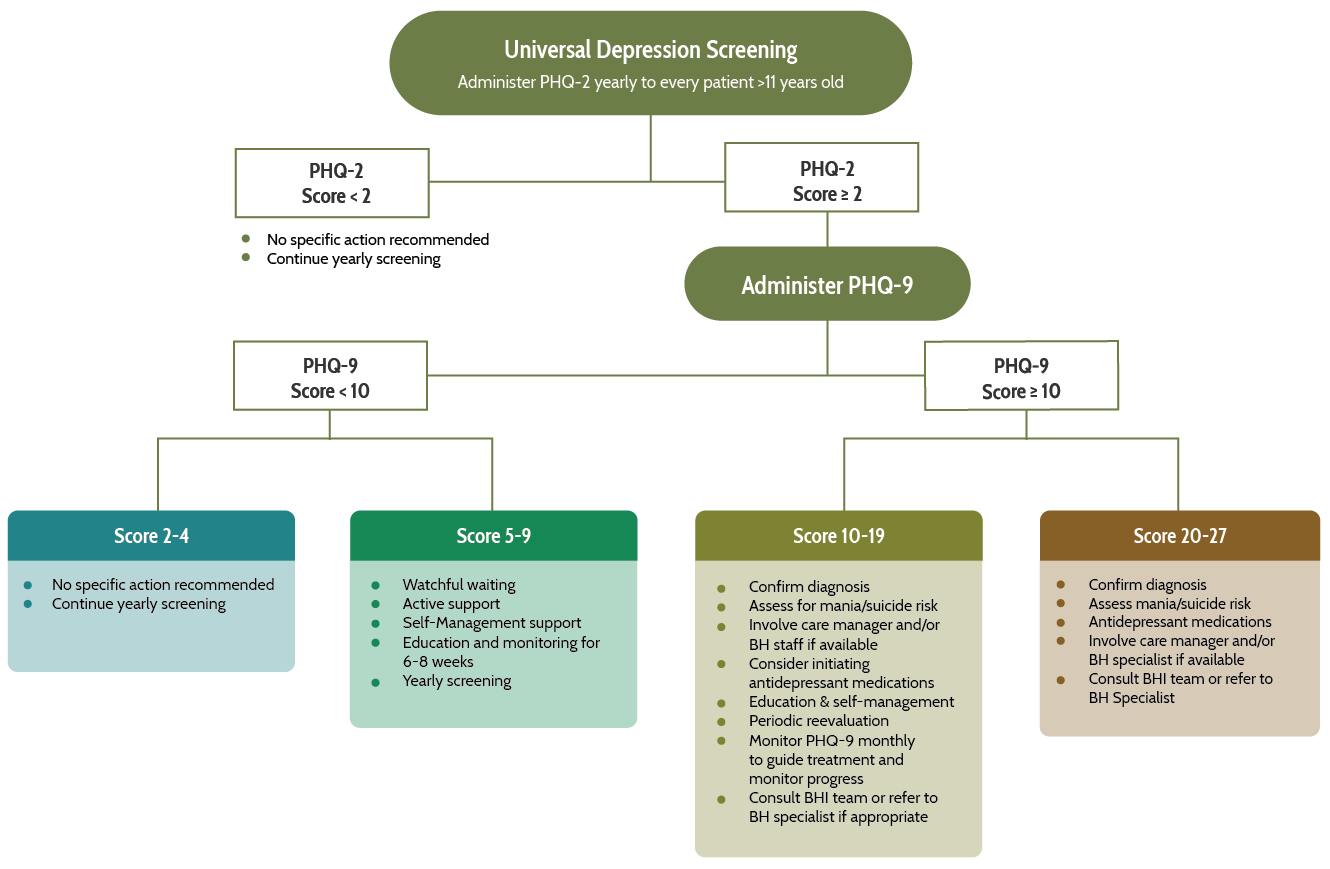
The PHQ 2 is a preliminary screening tool administered prior to the PHQ 9. Anyone who scores 2 or more on the PHQ 2 will need to have a PHQ 9 administered and a clinical evaluation to confirm or rule out a diagnosis of depression.
Who can administer the PHQ 2 and 9 to patients?
The PHQ 2 and 9 are useful tools for integrated care settings, as they can be administered by a variety of different staff and can be used with different approaches. The PHQ 2 and 9 should be completed by the patient, usually in the waiting room, and then scored by a staff person. Often administrative staff, medical assistants, care managers or nursing staff will score this form and subsequently enter the score into the electronic health record. In cases where patients have difficulty with reading or comprehension, a staff member can assist the patient in completing the tool. Assistance with completing the tools can be provided by any level of staff who has been trained in understanding the purpose and importance of the PHQ tools and in strategies for engagement and completion of the tools.
A score of 10 or above and/or a positive answer on question 9 of the PHQ 9, which is a screening for suicidal symptoms typically require further evaluation and a clinical intervention by the primary care provider, care manager or BH staff in the practice or via referral 3,4. A workflow will need to be developed to identify appropriate staff responsibilities and procedures for responding to these scores. This workflow includes review by the team (primary care provider, care manager and behavioral health staff, if available). Patients receiving intervention should be provided with regular follow up and tracked for improvement in their PHQ 9 score. The administration of the PHQ for follow up can be done in person, using phone calls and/or a smartphone application5,6. Results from studies that have analyzed telephonic and electronic administration of the tool have demonstrated that these methods yield similar results to being administered in person.
In which populations should the PHQ 2 and 9 tools be used?
The PHQ 2 and 9 are appropriate to be used with individuals 12 years of age and older. Alternative screening tools have been developed and validated for use among special populations including youth and older adults. These alternative tools can be accessed at: https://aims.uw.edu/resource-library/phq-9-depression-scale.
How often should the PHQ 2 depression screening tool be administered?
The U.S. Preventive Services Task Force (USPSTF) recommends screening for depression in adolescents ages 12 – 18 and in adults, including pregnant and postpartum women. “Screening should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up.”7 The American Academy of Family Physician recommendations mirror those of the USPSTF.8 The American Academy of Pediatrics recommends depression screening for adolescents beginning at age 11.9 At this time, there is no definitive guidance on how frequently someone should be screened for depression. The USPSTF states: “The optimum interval for screening for depression is also unknown; more evidence for all populations is needed to identify ideal screening intervals. A pragmatic approach in the absence of data might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted.”10 Certain populations with higher risks for depression, such as those with HIV infection, may be considered for regular screening. For example, the NY State AIDS Institute HIV guidelines recommend screening “for depression as part of the annual mental health assessment and whenever symptoms suggest its presence.”11 There is growing consensus that screening using evidence-based tools like the PHQ 9 is a critical component of delivering integrated care.
What does AHP recommend?
The AHP Behavioral Health Integration (BHI) team recommends screening for depression in individuals ages 12 and over at least once yearly. Peripartum women should be screened at least once during their pregnancy and postpartum period. Individuals who score positive on the PHQ 9 (score 10 and above) should be screened again every 4 weeks to assess their progress and guide their treatment. It is important to note that although the recommendation is to perform a follow up screen every 4 weeks, patients may need to be have follow up visits in person or by phone more frequently. This is particularly true in adolescents with depression.12 Clinical judgement should always guide the frequency of follow up in depression.
The frequency of PHQ 9 screening usually reverts back to yearly after 2 consecutive screens are deemed negative (score below 5).
Interpretation of the PHQ 9 scores and recommended actions.
Each item on the PHQ 9 is rated on a 4-point scale (0=Not at all; 1=Several days, 2=more than half the days; and 3=Nearly every day). The total score can range from 0 to 27, with higher scores indicating greater severity of depression. As a screening instrument, the PHQ 9 cannot replace sound clinical judgment. Before deciding on treatment, the clinician must carefully evaluate those with scores indicative of depression for coexisting situational issues such as suicidal thoughts; substance use; medical illnesses presenting with anergy, insomnia, or anorexia; or other comorbid psychiatric condition.13